Infusion Therapy For Psoriatic Arthritis
Living with psoriatic arthritis is painful and uncomfortable and for some people, it can be embarrassing. The condition occurs when your immune system attacks healthy cells, causing inflammation of the joints and the areas where tendons and ligaments connect to bones as well as overproducing skin cells. While the cause is unknown, people whove experienced a bacterial or viral infection may develop psoriatic arthritis if they already have a family history of the condition. Although psoriatic arthritis has no cure, you can obtain treatment to alleviate pain and preserve your joints range of motion.
Is There Any Way To Slow Down Its Progression
While theres no way to reverse or cure psoriatic arthritis, there are several things you can do to slow its development. These tend to work best when started earlier rather than later. You may want to consider seeing a rheumatologist as well. This is a type of doctor that focuses on autoimmune conditions.
The first step in slowing down psoriatic arthritis is controlling joint inflammation. There are several types of medication that can help with this, including:
- Nonsteroidal anti-inflammatory drugs . NSAIDs, such as ibuprofen and naproxen , are a good starting place because theyre available over the counter. They help reduce inflammation and pain.
- Cortisone injections. Cortisone injections target inflammation in a single joint. They work quickly to reduce pain and swelling.
- Disease-modifying antirheumatic drugs . DMARDs, such as methotrexate , leflunomide , and sulfasalazine , work to slow the progression of psoriatic arthritis. While this can help to prevent permanent joint damage, these drugs have many potential side effects.
- Biologic agents.Biologics are a new generation of arthritis medications that use genetic engineering to target inflammation in the body. They can slow down the progression of psoriatic arthritis and prevent joint damage.
If you have psoriatic arthritis, its also important to avoid putting added stress on your joints. This can involve:
Will There Ever Be A Cure For Psa
The experts were hopeful that a cure may someday be available, but they emphasized that there is still a lot that we need to understand before we can reach that point.
Ideally, a cure is the ultimate goal hopefully we can get there, Dr. Kavanaugh said. But PsA, like many autoimmune diseases, is incredibly complicated.
Drs. Merola and Perez-Chada agreed. A cure for PsA remains aspirational at present. However, the remarkable advances in genomics, informatics, immunology, molecular biology, and treatments are certainly paving the way toward finding a cure.
can get involved in research endeavors related to a cure and remission through multiple organizations dedicated to psoriatic research, suggested Drs. Merola and Perez-Chada.
These organizations include the:
Also Check: Are Eggs Bad For Psoriatic Arthritis
How Psoriatic Arthritis Treatment Prevents Disease Progression
The primary way to slow the progression of PsA is through medications that modify the immune system. It may take trial and error to find the treatment that works best for a given patient, notes Dr. Haberman. While we have a lot of medication options for PsA, we dont know which ones a patient will respond to, so sometimes we need to try more than one medication to find the one thats right for that patient, she says.
In addition, medications that have been effective for you can stop working over time. If this happens, your doctor may recommend a medication that works differently say, targets a different part of the immune system to control disease activity.
There are many drugs used to treat PsA. The ones that you will use will depend on the type and severity of symptoms as well as the most problematic areas .
Medications use to treat PsA include:
The Right Treatments Could Lead To Some Much Needed Relief

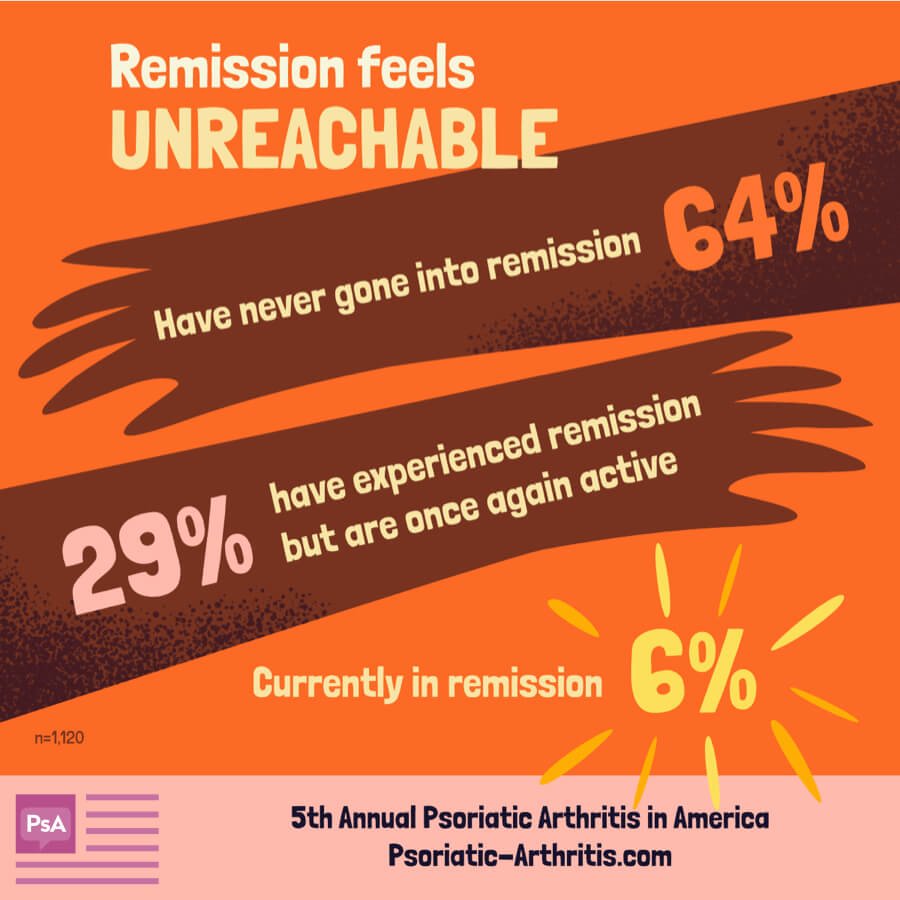
If you have psoriatic arthritis , you might worry that your painful, swollen joints will never be normal again. But the good news is, with the right treatment many people with PsA can achieve remission. One study showed that nearly two-thirds of subjects had minimal symptoms with 12 months.
What is remission? Remission means the disease is controlled says rheumatologist Paula Rackoff, MD, associate professor of clinical medicine at NYU School of Medicine. Patients in remission have minimal joint pain and stiffness. Theyre able to do all their daily activities with minimal symptoms and minimal morning stiffness.
Dr. Rackoff says that most people achieve remission from PsA within about six months. Once remission is achieved, Rackoff says that doctors usually try and see the least amount of medications that control the symptoms.Corticosteroids and disease-modifying antirheumatic drugs are most often prescribed by doctors to control symptoms.
Between 5 and 10 percent of people can come off medication entirely, according to Rackoff, and she adds that doctors generally wont start tapering medication until after about a year.
We always encourage people to exercise and strengthen the muscles around the joints that are affected, says Rackoff. The stronger the muscles are around a joint, the less the joint has to do.
Read Also: Acute Arthritis Symptoms
How Psa Is Currently Treated
At the end of 2018, NPF, in partnership with the American College of Rheumatology, released a pioneering treatment guideline for PsA. For the first time, doctors who care for people with PsA have a guide to all current treatments and the evidence-based recommendation to use biologics as a front-line treatment, before oral systemics.
The guideline adopted a âtreat to targetâ approach for PsA: The doctor and patient set targets for improvement and change how they manage the patientâs disease if targets arenât met. The guideline also includes evidence that patients can benefit from âself-managementâ: diet, exercise, lifestyle and physical therapy.
âFor us, at least in psoriatic arthritis, we have so many more treatments than when I was in medical school in the â90s. All we had then was methotrexate ,â Husni says. âItâs been really great to be able to have all these tools in my toolkit to use more individualized treatments. We have so many more treatments that are really working well, and allowing people to go back to their jobs, allowing people to go back to being active with their families.â
The most common treatments for PsA are biologics, oral treatments and, at times, off-label use of systemic therapies indicated for other inflammatory conditions. Biologics are made from living sources, such as human, animal or bacteria cells. They are given as injections or intravenous infusions.
Early Stages Of Psoriatic Arthritis
Recognizing the signs of psoriatic arthritis can be tricky since symptoms differ from patient to patient. For example, one person can experience psoriasis skin involvement and peripheral arthritis, another may experience axial disease , and someone else could have a combination of all three.
Whats more, especially during early disease, you may confuse your symptoms with other conditions. People can mistake enthesitis, inflammation of the entheses for tennis elbow or dactylitis for an infection, explains Dr. Mikulik.
If you have psoriasis and are having pain in your tendon and musculature and you think maybe Ive been too active lately, that may be the first sign of PsA, says Dr. Haberman. Doctors commonly hear people chalk up their symptoms to overuse, such as getting more exercise than usual or doing work around the house.
If you experience any of the following signs of early psoriatic arthritis its important to see your doctor as soon as possible:
- Back pain
- Changes in your fingernails or toenails, including holes, pitting, discoloration, or softness
- Eye inflammation
- Sausage-like swelling of an entire finger or toe
- Scalp psoriasis
- Skin rash
- Tendon or ligament pain at the Achilles tendon, bottom of the foot , or elbow
Read Also: How To Deal With Arthritis
Is There A Cure For Psoriatic Arthritis
There is no known cure for PsA, although there are several treatment options that can help, and in some cases, provide remission. Remission implies the reversibility of functional impairment, minimal or no progression to joint destruction, and, at least in theory, potential to heal a damaged joint. Recent research suggests remission is possible with anti-TNF therapy, which targets tumor necrosis factor .2 Tumor necrosis factor is a cytokine or chemical messenger, that is released by the white blood cells called T lymphocytes. TNF triggers multiple actions in the body, including the ability to induce necrosis of tumor cells. It also produces a wide range of inflammatory actions, such as those seen in PsA.3,4
A recent study indicated as many as 58% of PsA patients receiving treatment with an anti-TNF therapy experienced remission at 12 months. Several patient characteristics were predictors of remission, including patients of male gender and those with early morning joint stiffness. This does not conclude that female patients cannot achieve remission simply that remission was more likely to occur in male patients in this study.2
Myth : Biologics And Newer Drugs Are Only For Severe Cases
Biologic drugs are disease-modifying, which means they stop or slow disease by calming specific parts of the immune system. The immune system is pretty broad, and there are multiple cells and cytokines that lead to joint pain and joint swelling, says Luk. By blocking some aspects of the immune system, he explains, biologics can ease psoriatic arthritis symptoms and even prevent bone damage and joint damage.
Also Check: How To Deal With Arthritis
Are There Any Other Alternative Approaches
There are a variety of alternative approaches that can be undertaken alone or in combination with conventional therapies. It is essential if you are considering any alternative approaches to please discuss this with your doctor or healthcare professional as they may be detrimental to your health.
Such alternative approaches could entail Chinese Medicine, Acupuncture, Magnatherapy, Ayurvedic Medicine, Aromatherapy, Homeopathic Medicine, Yoga, Spa Treatments, Shiatsu, and Naturopathy. It is always advisable to fully research and find a reputable qualified practitioner who follows correct protocols for their clients. There are organisations that may be useful to contact for further details and advice. With this information you and your doctor or healthcare professional will be better placed to discuss what is best for you.
Myth : You Can Stop Psoriatic Arthritis Treatment When You Start Feeling Better
Most rheumatologists recommend that you stay on your medication even after you reach remission, according to the Arthritis Foundation. Unfortunately, if people stop taking their medicines, the psoriatic arthritis will probably come back, says Luk.
Matteson agrees, saying that only a small percentage of people with psoriatic arthritis who reach remission are able to stop taking their medication completely. Most people find that their disease flares up again, he says. A study published in 2017 in the Journal of Rheumatology found that rebound disease activity returned for 73 percent of people who stopped their tumor necrosis factor inhibitor, the first-line biologic therapy for psoriatic arthritis. These findings support those of other, smaller studies.
Read Also: How To Deal With Arthritis
What Are The Trigger Factors
Although the underlying cause of psoriasis stems from your body’s immune system, the trigger factors that can make it worse or cause flare-ups include:
- Weather: Cold and dry weather can dry out your skin, which makes the chances of having a flare-up worse. In contrast, hot, sunny weather appears to help control the symptoms of psoriasis in most people
- Stress: Having psoriasis can cause stress itself and patients often report that outbreaks of symptoms come during particularly stressful times
- Some medications: Certain drugs, such as lithium , drugs for malaria, and some beta-blockers , can cause flare-ups of psoriasis. Some common painkillers — called non-steroidal anti-inflammatory drugs — may also aggravate psoriasis, although they are still used in some people with psoriatic arthritis
- Infections or disease: Certain infections, such as strep throat or tonsillitis, can result in guttate or other types of psoriasis. Psoriasis may worsen in people who have HIV
- Trauma to the skin: In some people with psoriasis, trauma to the skin — including cuts, bruises, burns, bumps, vaccinations, tattoos and other skin conditions — can cause a flare-up of psoriasis symptoms either at the site of the injury or elsewhere. This condition is called Koebner’s phenomenon
- Smoking: Some experts think that smoking can worsen psoriasis.
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
Also Check: Arthritis Symptoms In Leg
Lifestyle And Home Remedies
- Protect your joints. Changing how you do everyday tasks can make a difference in how you feel. For example, use gadgets such as jar openers to twist the lids from jars, lift heavy objects with both hands and push doors open with your whole body instead of just your hands.
- Maintain a healthy weight. This places less strain on your joints, leading to reduced pain and increased energy and mobility. Losing weight if needed can also help your medications work better. Some psoriatic arthritis medications are less effective in people who are overweight.
- Exercise regularly. Exercise can help keep your joints flexible and your muscles strong. Types of exercises that are less stressful on joints include biking, swimming, walking, yoga and tai chi.
- Stop smoking. Smoking is associated with a higher risk of developing psoriasis and with more-severe symptoms of psoriasis.
- Limit alcohol use. Alcohol can decrease the effectiveness of your treatment and increase side effects from some medications, such as methotrexate.
- Pace yourself. Battling pain and inflammation can leave you exhausted. In addition, some arthritis medications can cause fatigue. Don’t stop being active, but rest before you become too tired. Divide exercise or work activities into short segments. Find times to relax throughout the day.
Talk With Others Who Understand
MyPsoriasisTeam is the social network for people with psoriasis and their loved ones. On MyPsoriasisTeam, more than 91,000 members come together to ask questions, give advice, and share their stories with others who understand life with psoriasis.
Is your psoriasis currently in remission? Share your experience in the comments below or start a conversation by posting on MyPsoriasisTeam.
You May Like: Test For Arthritis In Knees
What Is The Genetic Predisposition
Genetic predisposition means an inherited tendency to develop the disease. Recent research has greatly increased our knowledge about how and what we inherit from our parents and the role played by genes. As our knowledge increases so does our appreciation of the complexity of the process. While it was originally hoped that a specific disease might be associated with a specific gene, it now appears that for many diseases that have a genetic component, including psoriasis, there are probably multiple genes involved in producing the sequence of events that results in the expression of disease. This is further complicated by the way these genes interact.However, the evidence to support the belief that a genetic predisposition plays a major role in the cause of psoriasis can be summarised as follows:
- One third of people with psoriasis have a family member who is also affected
- There is an increased incidence of psoriasis in children when one or both parents have the disease
- In twins, psoriasis is more likely to appear in both identical twins than in both non-identical twins. This finding also confirms that more than one gene must be involved.
Focusing On People With Psoriasis
Most people with psoriatic arthritis have psoriasis first. For a small percentage of patients, psoriatic arthritis occurs before psoriasis, although most often they will have a first-degree relative with skin psoriasis, notes Dr. Haberman. Still, others have no skin psoriasis or dont notice the psoriasis hidden in areas like the scalp, umbilicus, and gluteal fold.
Read more about the connection between psoriasis and PsA.
Up to 30 percent of patients with psoriasis will go on to develop psoriatic arthritis, says Dr. Haberman. The majority of cases begin with the skin condition and then progress to joint pain within seven to 10 years. Recent studies have found that patients with psoriasis who develop severe fatigue, heel pain, and joint pain without overt swelling are more likely to develop PsA.
While we dont yet know which individual patients with psoriasis will go onto develop PsA, researchers have identified a few potential risk factors for the progression of PsA, including:
- Family history of psoriatic arthritis
- Psoriasis that affects the scalp and groin
- Nail involvement in psoriasis, such as nail pitting
- Being overweight or obese. PsA is worse in patients who are overweight and often biologics may not work as effectively in people who are overweight, says Dr. Haberman.
- Smoking
- Age
- Exposure to certain infections
- Physical trauma
Don’t Miss: Over The Counter Medicine For Rheumatoid Arthritis
Myth : Nsaids Are Risk
NSAIDs are commonly used to relieve joint pain, stiffness, and inflammation in people with psoriatic arthritis. Certain versions are available over the counter, like ibuprofen, while stronger forms require a prescription. For mild cases of psoriatic arthritis, NSAIDs can be helpful, Matteson says. Theyre for the management of pain. They dont change the course of the disease.
But though doctors prescribe NSAIDs for milder psoriatic arthritis symptoms, that doesnt mean these drugs dont have risks or side effects. They do have risks, Matteson says. This can include stomach bleeding, hypertension, or kidney damage, especially if used at higher doses for long periods of time. Be sure to discuss these risks with your physician.
Myth : Most People With Psoriatic Arthritis Eventually Require Surgery
Whether or not youll need surgery depends on many factors, including how early you get a diagnosis and how aggressively doctors treat your disease.
The good news is that most people with psoriatic arthritis wont ever have to have surgery, according to the Cleveland Clinic in Ohio, and should be able to manage the disease through a combination of medications and lifestyle modifications.
But if psoriatic arthritis has severely damaged your joints, your doctor may recommend surgery to relieve pain and restore function.
Additional reporting by Becky Upham.
Don’t Miss: What Does Ra Pain Feel Like